At Ormiston Hospital, we have a highly skilled team of gynaecologists who diagnose, treat, and provide preventative care for these conditions, and who work with our patients’ specific needs based on their different stages of their life. The specialists at Ormiston Hospital are passionate about women’s health and provide a leading service in state-of-the-art facilities. Our services are dedicated to maintaining overall reproductive health, and include regular check-ups, screenings, and various treatment options tailored to each patient.
Our range of available procedures include:
Endometriosis:
Endometriosis is a medical condition in which tissue that looks like the lining of the uterus, grows outside the uterus. This can cause painful and heavy periods leading to fertility issues. While mild cases can be managed with medications, in severe cases, surgical options such as laparoscopy and hysterectomy are recommended.
Operative Hysteroscopy:
Operative hysteroscopy is a minor surgery that is used to treat abnormal uterine bleeding, heavy menstrual bleeding, and bleeding after menopause. During this procedure your surgeon will use a device to remove the abnormalities.
Ovarian Cysts:
Ovarian cysts are common growths that develop on or inside the uterus. Most of them are benign (non-cancerous) and painless, but a few can cause serious symptoms. They are removed by a procedure called laparoscopy, in which an instrument called laparoscope is inserted into your abdomen to perform the procedure. The surgeon removes the cyst by making small cuts in your skin.
Pelvic Organ Prolapse (POP):
Pelvic organ prolapse is a condition where one or more organs in the pelvis such as the uterus, vagina, bladder, and rectum sag (prolapse) due to weakening of the muscles in the pelvis. In severe cases, an organ bulges into another organ and sometimes, outside the body as well. It can be treated with pelvic floor exercises, vaginal pessary (a detachable silicone device your doctor will insert into the vagina to hold a prolapsed organ in place) and surgery is recommended in severe cases.
Other gynaecological procedures:
- Menstrual problems—absence of periods, heavy bleeding, irregular periods
- Urinary tract diseases and pelvic floor dysfunction (urogynaecology)
- Laparoscopy—viewing internal organs of the female reproductive system, diagnosing and treating infections and cysts in the ovaries and fallopian tubes
- Colposcopy—viewing the insides of uterus using an instrument called a colposcope
- Adolescent gynaecology
- Post-pregnancy problems
- Menopause
- Cervical screening
- Vulvar diseases/disorders
- IUD fitting
Need to know
You should consult a gynaecologist when you experience:
- Heavy bleeding during menstruation
- Irregular periods
- Complete absence of periods
- Bleeding after menopause
- Unexplained vaginal bleeding
- Bleeding between periods
- Itching or burning sensation
- Discomfort or extreme pain in your abdomen
During your private consultation with one of our gynaecologists, they may ask a few questions about your current health condition and medical history. They may perform a physical examination as well. They will provide advice, perform some tests, and diagnose your condition. After assessing your condition, they will suggest a treatment plan. If you wish to proceed with treatment, you can then work with the admissions team to schedule the procedure.
To prepare for the surgery, it is important to follow your surgeon’s specific instructions. It is also important to arrange for someone to drive you home post-surgery and to plan for a recovery period at home.
During the surgery, the specific steps depend on the type of procedure being performed. Generally, you will be given anaesthesia — either local, where only the surgery area is numbed, or general, where you are asleep during the operation. Throughout the surgery, your vital signs are closely monitored for safety, and the surgical team ensures that the procedure is as smooth and efficient as possible.
After surgery, you will be taken to a recovery area where medical staff will monitor your vital signs and ensure you’re recovering well from the anaesthesia. Your doctor will provide instructions and medication to help manage pain and advice on when you can resume normal activities. There will also be one or more follow-up appointments so your doctor can monitor your healing process.
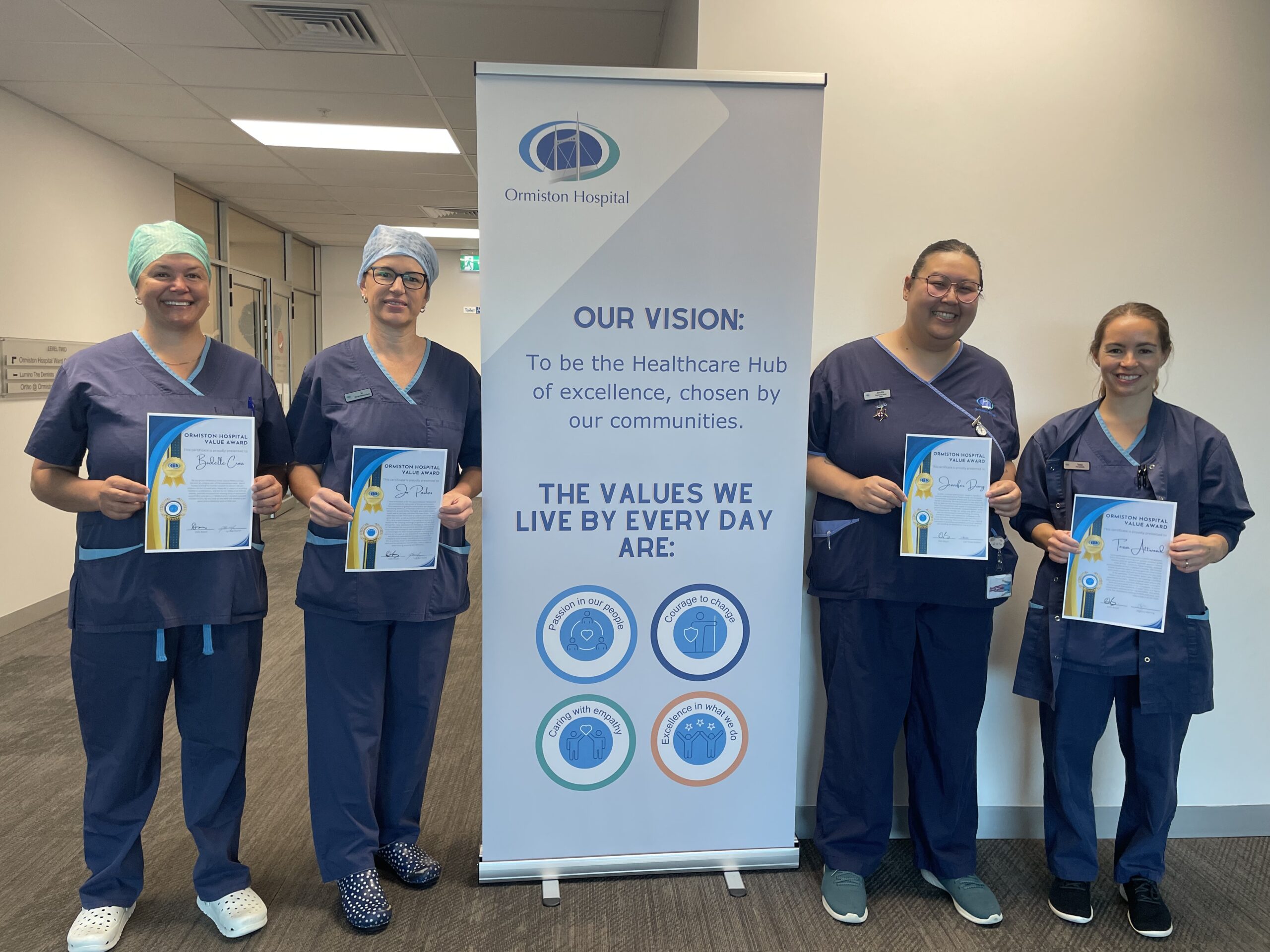
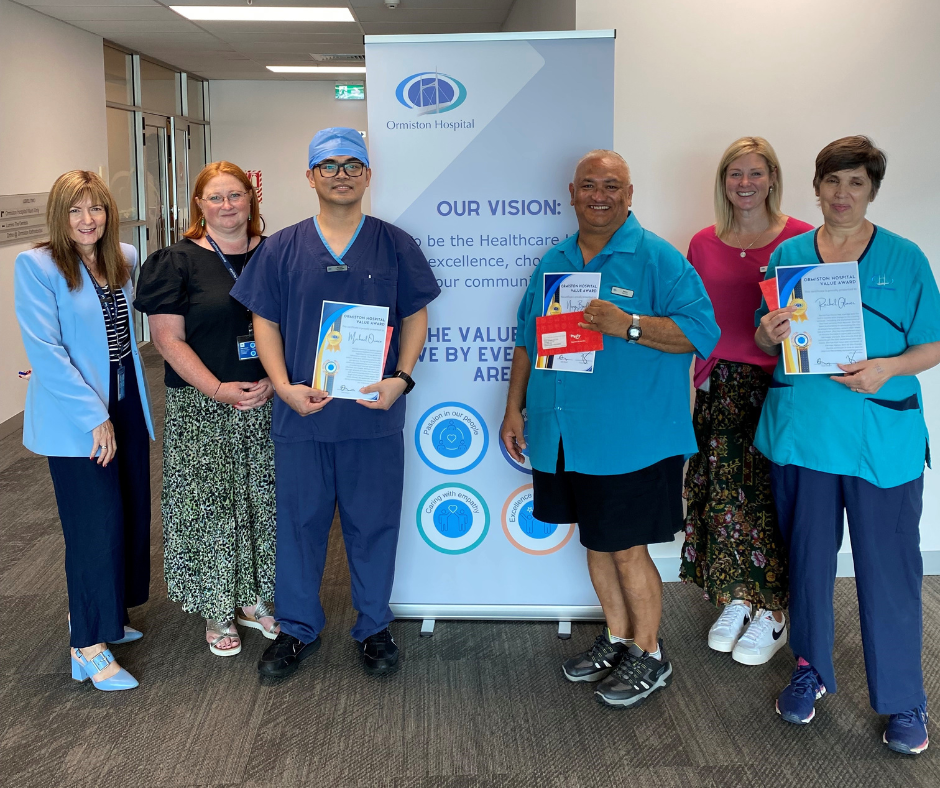
Specialist Surgeons